Running outdoors is an incredible way to get some fresh air, exercise and squeeze in a well-deserved mental break after a long workday. As spring emerges, many people will dust off their old runners and hit the trails. It is important to start slowly and build up towards your fitness goals. Try not to compare your current performance to your ability at the end of last summer. This will set you up for disappointment. Start slow and each day push a little harder and run a little further. As the old saying goes: ‘it’s a marathon, not a sprint.”
Regardless of your motivations for getting active, you will likely experience fatigue and injury along the way (to varying degrees). Three repetitive running injuries that we commonly treat include patellofemoral pain syndrome (runner’s knee), shin splints and plantar fasciitis. These conditions can be brought on by a sudden increases in training frequency, intensity or duration (“too often, too fast and too much”). Self-management techniques go a long way towards preventing these injuries. Carefully plan your workouts allowing for adequate rest between sessions accompanied by appropriate nutrition. Make sure you stretch before every workout and maintain optimal form while running.
Patellofemoral Pain Syndrome (PFPS):
Patellofemoral pain syndrome (PFPS) accounts for 16-25% of all running injuries. It is described as pain behind, underneath or around the kneecap and is aggravated by running, forceful or repetitive knee extension, squatting or jumping. Sometimes a popping sound, grinding sensation or mild knee buckling can occur. PFPS is a functional diagnosis and is considered after more serious injuries are ruled out. PFPS is associated with three major contributing factors:
a) Malalignment of the lower limb or knee cap (“poor knee tracking”)
b) Muscular imbalance around the knee (especially quadriceps-hamstring strength ratio)
c) Overactivity (eg. increased running/cycling mileage)
A basic principle in physical therapy is to identify the contributing factors of a condition, and to use those to guide treatment. Therefore, treatment for PFPS aims to improve knee tracking, optimize muscle balance around the knee and alter your current activity levels. Activities like squatting, kneeling, cycling with a low seat or excessive running should be avoided. Treatment may include any combination of RICE principles (rest, ice, compression and elevation), strength training, stretching, Kinesiotape or athletic tape, soft tissue therapy, NSAID’s, gait retraining, knee braces and/or prescription orthotics. At the[fix], we use 3D Gaitscan technology to analyze your gait and cast you for custom fit orthotics. Orthotics are covered by most insurance plans.
Shin Splints (Medial Tibial Stress Syndrome):
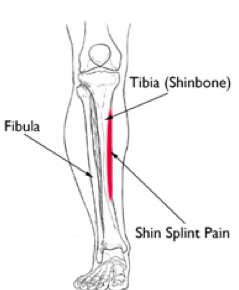
Shin splints produce a vague, diffuse pain along the inside of the shinbone (tibia). Recently, shin splints has become a catch all term to describe any type of shin pain. Tibialis anterior strains get incorrectly grouped in with shin splints even though they occur on the opposite side of the tibia. True shin splints happen on the INSIDE of the tibia rather than the outside.
Repetitive muscle contraction of the tibialis posterior and flexor digitorum pull on their attachment to the tibia causing inflammation and micro-tearing at the bone surface. Having flat feet, high arches and wearing improper footwear can contribute towards this condition. It is important to differentiate shin splints from stress fractures, chronic exertional compartment syndrome and acute tendonitis.
Self-management techniques for this condition include a combination of RICE principles, stretching, strength training, activity modification and ensuring proper footwear. Massage therapy, orthotics, acupuncture, taping and gait pattern analysis can help to relieve pain and improve recovery. At the[fix] we use a tailored combination of these treatment methods to ensure we are addressing your unique injury.
Plantar Fasciitis:
Plantar fasciitis is one of the most common foot complaints in athletic and non-athletic populations. The plantar fascia is a thick band of connective tissue that lines the base of the foot that connects your heel to the base of your toes to support your arches. Plantar fasciitis involves inflammation of the plantar fascia due to repetitive overuse. Pain is felt along the inside arch with focal pain towards the heel.
Poor running shoes and running on an uneven surface promotes the development of plantar fasciitis. Risk factors include prolonged standing, being flat-footed, poor ankle range of motion and heel spurs. Treatment includes a combination of massage therapy, intrinsic foot muscle and calf strengthening, taping, acupuncture and joint mobilization. Custom orthotics, night splints or gait retraining may also be warranted. If severe inflammation is present, then your medical doctor may prescribe anti-inflammatory medications. At the[fix], most of our patients respond well to a conservative treatment approach and are able to return to normal activity in a few months.
Conclusion:
Running is one of the best workouts you can do for overall heath. Make sure you take advantage of the beautiful sunshine because it only lasts a few months! Get outside and get healthy! Take preventative measures to reduce your chance of experiencing these common running injuries. Gradually build up the duration, frequency and intensity of your workouts. Logging your mileage and timing yourself are good ways to keep track of your progress. Make sure you are diligent with stretching and strengthening to prevent fatigue and injury. If you are experiencing any of these symptoms or would like advice, book an appointment today for an Initial Chiropractic Assessment and Treatment. During this visit we may recommend a combination of registered massage therapy, custom orthotics, exercise prescription and/or acupuncture in addition to comprehensive chiropractic treatment.
References:
AAOS. (2012). Otho Info: Shin Splints, The American Academy of Orthopedic Surgeons (AAOS). Updated: May 2012. Retrieved from: http://orthoinfo.aaos.org/topic.cfm?topic=a00407.
Buchbinder, R. (2004). Plantar fasciitis (Clinical Practice), New England Journal of Medicine, 350:2159-2166.
Galbraith, R. M., & Lavallee, M. E. (2009). Medial tibial stress syndrome: conservative treatment options. Current reviews in musculoskeletal medicine, 2(3), 127-133.
Mayo Clinic Staff. (2016). Plantar fasciitis: Patient Care & Health Information, Mayo Clinic. Retrieved from: http://www.mayoclinic.org/diseases-conditions/plantar-fasciitis/home/ovc-20268392.
Moen, M.H., Tol, J.L., Weir, A., Steunebrink, M., De Winter, T.C. (2009). Medial tibial stress syndrome: A critical review, Sports Medicine, 39(7):523-545.
Schiepsis, A.A., Leach, R.E. Gouyca, J. (1991). Plantar fasciitis: etiology, treatment, surgical results and review of the literature, Clinical Orthopaedics & Related Research, 226.
Thomee, R., Augustsson, J., Karlsson, J. (1999). Patellofemoral Pain Syndrome: A Review of Current Issues, Sports Medicine, 28(4):245-262.
![the[fix]](http://images.squarespace-cdn.com/content/v1/5494e530e4b039edeef75dff/1467052868801-4WDDECP8CV27LAFWPL65/the%5Bfix%5D+logo+TM.jpg?format=300w)